Staff Safety in 2026: Turning Panic into a Plan
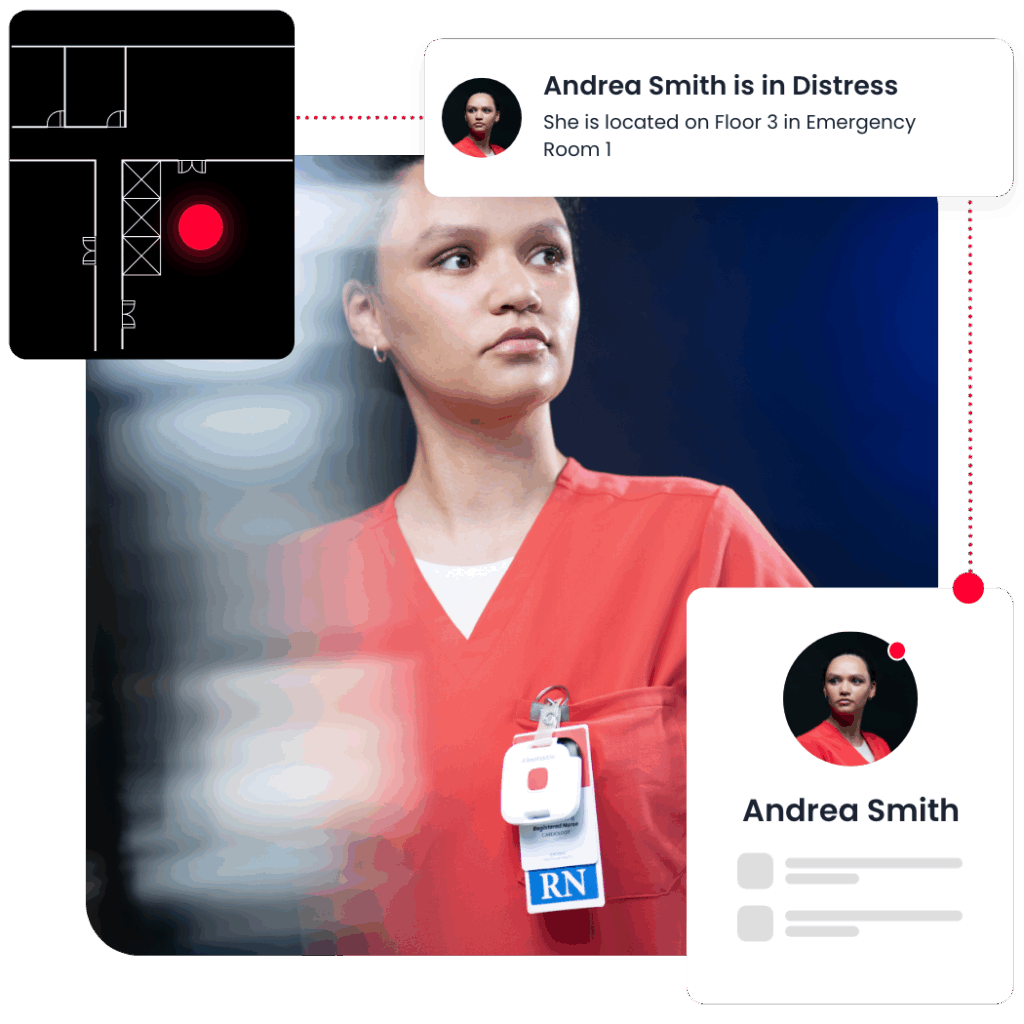
A charge nurse in a crowded ED presses a badge once. Within seconds, the nearest trained responders are already moving, one to the door and another to the bedside, guided by a quiet orchestration running beneath the hospital’s daily chaos.
No radio chatter, no guesswork about location, no delay at the elevator bank. The incident de-escalates before it becomes a headline.
That’s how staff safety should work in 2026 when it’s treated not as a gadget, but as infrastructure.
Why panic buttons are not enough
For years, hospitals bought “panic buttons for healthcare workers” and hoped for the best. They got alerts (sometimes) but not coordination. The gap wasn’t courage or policy. It was architecture. A wearable duress system that shouts “help” without telling who should go, from where, and with what context simply externalizes risk to the nurse at the bedside.
The fix is a health and safety platform that understands distance, role, training, and room conditions, and then quietly routes people and resources the way a good charge nurse already does in her head.
Why coordinating responses beats locating badges
This is the shift defining 2026: orchestration over notification. With a modern, open RTLS backbone (BLE for campus coverage and selective IR for room certainty) alerts become assignments. A badge press in Behavioral Health pulls the closest, appropriately trained responder, nudges Security to the correct entrance, and surfaces the right context at the moment of need: behavioral flags, sitter proximity, available equipment. In the ambulance bay and the parking structure, the same workplace duress technology follows the worker, not the walls.
For Chief Nursing Officers, the impact shows up where it matters most: calmer units, fewer escalations, and measurable relief from the everyday friction that fuels burnout. De-escalation techniques (early awareness, door-side positioning, calm choices, and short time boxes) work best when the system quietly sets the stage. When help arrives in under ten seconds and is prepared, nurses don’t carry the cognitive load alone. Over weeks, the familiar signs of burnout in healthcare workers, such as hypervigilance, fatigue, intent-to-leave, begin to recede because the work itself gets lighter and more predictable.
For Hospital IT and Security, the story is equally pragmatic. Safety becomes part of the hospital’s operating layer, not a silo. A cloud-first, open stack integrates with nurse call, incident systems, and the EMR via HL7, FHIR, and webhooks. Identity and access live where they should (think SSO and role-based access controls), while data are encrypted, audited, and exportable to the hospital’s lake house or SIEM. The hardware footprint stays refreshingly boring: battery-powered IR only where room certainty is clinically necessary; BLE everywhere else. Disposable edge devices mean swap, not repair. Cost becomes predictable with per-bed subscriptions that bundle software, hardware, batteries, swaps, warranties, and support. That’s not just easier to run; it’s also easier to fund.
How can hospitals implement a systematic approach to staff safety?
This approach, which creates a unified hospital platform for staff safety, asset visibility, patient flow, and hand hygiene, also changes how leaders talk about value. You’re no longer just reducing assault risk; you’re also reducing sitter overtime, reclaiming nurse minutes every shift, and shortening time-to-stabilize. In a med-surg unit, the same signals that route a response also help charge nurses balance assignments by distance and acuity. In the ED, incident timelines feed post-event huddles with facts instead of folklore. Capacity grows without adding headcount because the invisible travel time, the duplicate calls, and the scavenger hunts melt away.
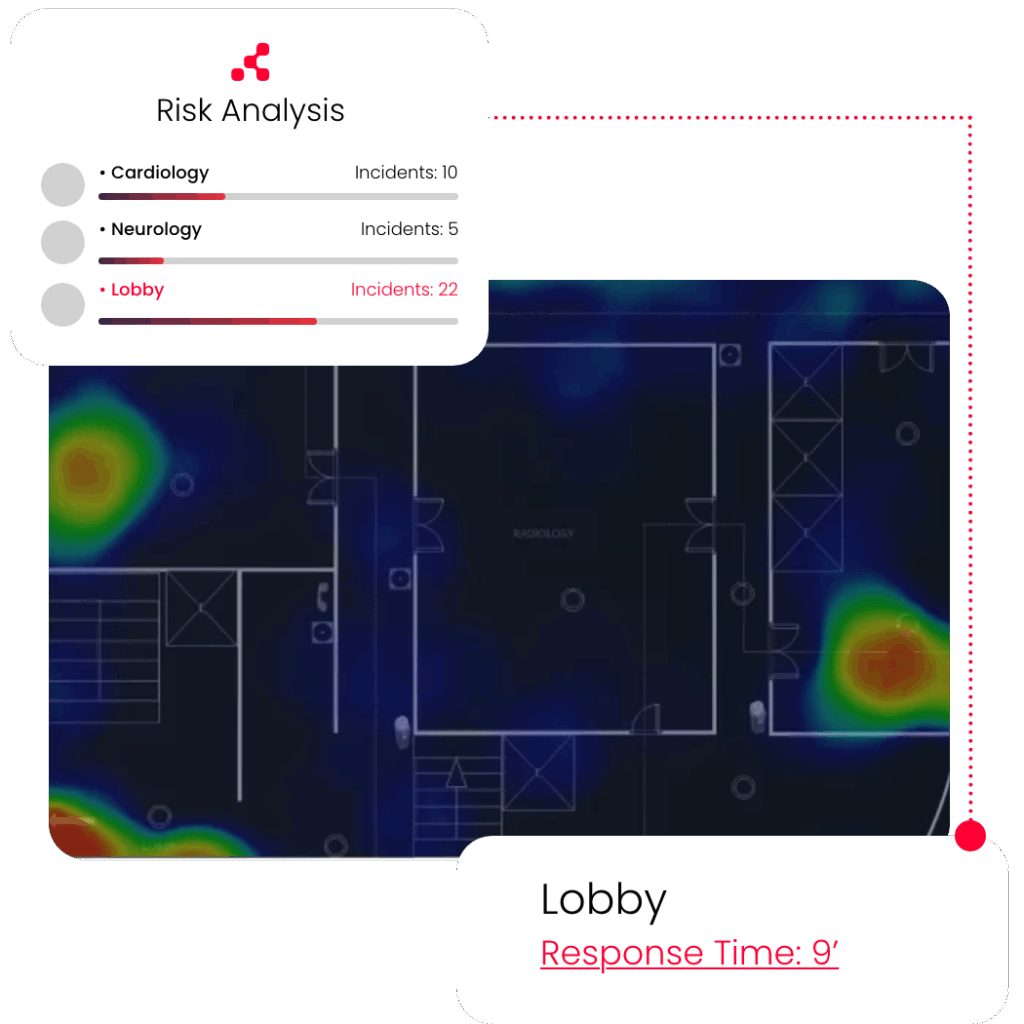
The path to outcomes is refreshingly short. Start where risk is highest (think ED triage, Behavioral Health, L&D triage) and design around a few hard metrics: alert-to-first-responder, time-to-resolve, incident density per 1,000 shifts, and close-out compliance. Stand up BLE campus-wide, place IR only where you truly need room-level certainty, and issue badges to the cohorts you want to protect first. Run short, shift-based drills that pair the staff duress technology with the de-escalation playbook you already trust.
Within a month, validate the real routes responders take, such as doors, elevators, and stairwells, and tune them. By the end of a quarter, publish the before-and-after on response times, escalation rates, and staff sentiment. Then take it outside the unit to parking lots, walkways, and ambulance bays, because hospital worker safety doesn’t stop at the sliding doors.
What staff safety looks like in 2026
Skeptics will ask whether a simpler “panic button” isn’t good enough. In a word: no. 2009-era RTLS thinking gives you hallway beeps and after-action spreadsheets. A modern, 2026-era safety mindset gives you workplace duress RTLS that knows the difference between zone and room, alert and assignment, or noise and signal.
This updated design philosophy also provides an open health and safety platform that your teams can build on. Even if you start with duress today, tomorrow you can easily move onto transport coordination, hand hygiene, or exam-room optimization, all without having to rearchitect any part of your environment. It’s how you move from incident management to operational maturity.
How do staff safety systems benefit hospitals and employees?
If you lead Nursing, this is about making help both faster and more certain. If you lead IT, it’s about integrating safety into the hospital’s digital nervous system: secure, interoperable, and boring in the best possible way. And if you lead both sides to the same table, you’ll discover that safety in the hospital is really about time, giving nurses back the minutes that convert stress into care.
In 2026, it’s no longer enough to ask, “Do we have panic buttons?” This approach is too limited; instead, the right question to ask is “Do we have a plan that runs itself?”
With an open, disposable, AI-orchestrated platform, the answer is a resounding yes.
