
Healthcare is a team sport played under pressure. When the field gets chaotic—unpredictable schedules, missing equipment, unsafe conditions—people burn out. This guide is for U.S. hospital leaders and frontline staff who are problem-aware and hungry for real solutions. It’s empathetic, practical, and focused on system-level fixes that create safer, more predictable care environments.
Executive Summary
- Burnout in healthcare is widespread and rising post-pandemic (CDC 2023; NAM). It’s driven by system conditions—understaffing, uncertainty, safety risks, and excessive manual work—not individual resilience gaps.
- The consequences hit patient safety, throughput, and financials—making burnout a strategic and operationalissue.
- Real progress comes from safer environments, visibility into demand and risk, reduced manual burden, and leadership feedback loops—with digital signals (RTLS, scheduling, simple analytics) used to prevent problems, not just find them.
What Is Burnout in Healthcare?
Burnout in healthcare is an occupational syndrome characterized by emotional exhaustion, cynicism (depersonalization), and a reduced sense of accomplishment. It’s not a personal weakness or a time-management issue. It’s a signal that the work system is failing the workforce.
By the Numbers (U.S.)
- U.S. Surgeon General’s Advisory (2022): Summarizes that physician demand will continue to outpace supply with a projected 54,100–139,000 physician shortage by 2033, and that even before COVID‑19, burnout had reached “crisis levels”—35–54% of nurses and physicians and 45–60% of medical students and residents reporting symptoms. (HHS, Surgeon General’s Advisory)
- Post‑pandemic reality: 46% of health workers reported feeling burned out often or very often in 2022. (CDC Vital Signs, 2023)
- EHR is not the differentiator: Burnout remains above pre‑pandemic levels regardless of EHR or organization. (KLAS Arch Collaborative, 2024)
Why this matters: Burnout directly affects patient outcomes, safety, and the bottom line. Treat it as a strategic, operational, and safety challenge – not just an HR concern.
What are Signs of Burnout in Healthcare Professionals
Burnout in healthcare rarely announces itself with a dramatic event. It builds quietly, shift after shift, when demand outpaces capacity and variability becomes the norm. For nurse managers, HR leaders, and clinical directors, recognizing early signals is the difference between proactive prevention and costly turnover.
Burnout is not just how someone feels. It’s how the system is performing.
Persistent Emotional Exhaustion
Staff dread upcoming shifts. Recovery doesn’t happen after days off. Irritability and emotional numbness increase. This isn’t normal fatigue—it’s sustained system overload.
Detachment and Cynicism
Reduced empathy, withdrawal from teamwork, or “nothing changes” language are classic burnout markers. Cynicism is often a protective response to unpredictability or feeling unheard.
Rising Errors and Slower Response
Burnout impairs attention and decision-making. Watch for near-misses, documentation gaps, delayed medication administration, or slower response times. These are capacity warnings—not competence failures.
Workforce Instability
Increased absenteeism, last-minute shift swaps, internal transfers, and exits citing “work environment” are leading indicators of burnout in healthcare. Turnover is the lagging metric.
Operational Chaos
Repeated equipment scavenging, delayed OR starts, unready rooms, or escalating safety incidents signal system strain. Reliability breakdowns and staff burnout are tightly linked.
Top 5 Reasons for Burnout in Healthcare Workers
Chronic Understaffing and Unmet Demand
Fewer hands, more patients. Volume spikes and acuity mix changes without matching staffing cause sustained overload.
Uncertainty and Unpredictability
Staff walk into shifts unsure whether rooms, equipment, or coverage will be ready. Constant fire-drills and last-minute changes drain capacity.
Safety Risks and Workplace Violence
When staff don’t feel physically and psychologically safe, stress skyrockets. Delayed or unclear response to duress events erodes trust.
Excessive Manual Work and Interruptions
Searching for mobile medical equipment, double‑documenting, phone tag with transport/EVS—minutes become hours. This is where healthcare worker burnout solutions have the fastest ROI.
Leadership Gaps and Misaligned Incentives
If leaders measure only cost and not capacity, reliability, or safety, the system produces burnout by design. Frontline teams read that signal loud and clear.
How to Prevent Healthcare Worker Burnout
Prevention is about designing predictable, supportive work environments. Individual coping helps, but systems change is what sticks. Here are five principles that can help to prevent burnout in healthcare.
1. Make Safety Non‑Negotiable
Room‑level duress coverage, rapid response routing, and clear post‑incident follow‑up. People can’t deliver compassionate care if they don’t feel safe.
2. Stabilize the Workday
Improve schedule reliability and on‑time starts. Use real‑time signals to confirm room readiness, equipment availability, and staffing coverage before a shift begins.
3. Reduce Manual Burden
Automate low‑value tasks (e.g., bed turnover triggers, supply distribution, documentation timestamps). Every nurse hour given back is capacity you don’t need to hire.
4. Visibility Over Heroics
Give leaders and charge nurses live views of demand, risk, and bottlenecks. Predictive insights beat post-hoc reports. Leadership should narrate these changes in huddles so staff see problems addressed, not ignored.
5. Close the Loop
Build feedback from frontline to leadership. When staff report a hazard or workflow failure, they should see how it’s fixed and when.
These principles align with preventing burnout in healthcare by treating variability and uncertainty as design problems – not staffing “attitude” problems.

The Hidden Costs of Staff Burnout in Healthcare
Burnout in healthcare is not just a workforce wellbeing issue, it is a measurable operational and financial liability. When clinicians operate in sustained overload, the impact spreads beyond individual stress. It affects patient safety, throughput, culture, and long-term financial performance. Hospitals often absorb these costs indirectly through delays, turnover, and declining quality metrics, without labeling burnout as the root cause. But make no mistake: staff burnout is expensive when it ties to what it leads to.
Patient Safety and Quality
Burnout correlates with higher error rates, delayed care, and communication breakdowns. Unpredictable OR starts or missing equipment cascade through the hospital day.
Cost of Hiring a New Person
Replacement costs for a bedside nurse can exceed annual salary when onboarding, traveler coverage, and productivity dips are included. Chronic turnover preserves chaos.
Worse Team Morale and Culture
Unsafe or unreliable environments normalize workarounds and erode accountability. High performers leave first.
Long‑Term Performance
Hospitals running on heroics miss growth opportunities, struggle with throughput, and suffer from poor HCAHPS and safety grades—hurting payer mix and revenue.
What Frontline Workers Can Control to Reduce The Burnout
Let’s be honest: you don’t control the budget or the schedule. But you do have levers.
- Name it early. If you notice rising irritability, detachment, or error risk, escalate. Early disclosure is professional, not personal.
- Use safety tools. Wear your duress badge, log incidents, and insist on follow‑up. Safety is a right.
- Lean on peers and charge nurses. Fast debriefs after tough events; ask for relief coverage when you’re at capacity.
- Document hazards. If a room is repeatedly unready or a unit is routinely understaffed, log it. Patterns drive change.
Individual strategies help, but they cannot replace system redesign. Leaders must fix the environment.
Practical Solutions to Reduce Healthcare Burnout
This is where technology and leadership meet outcomes. Think categories, not products:
Safer Physical & Psychological Environments
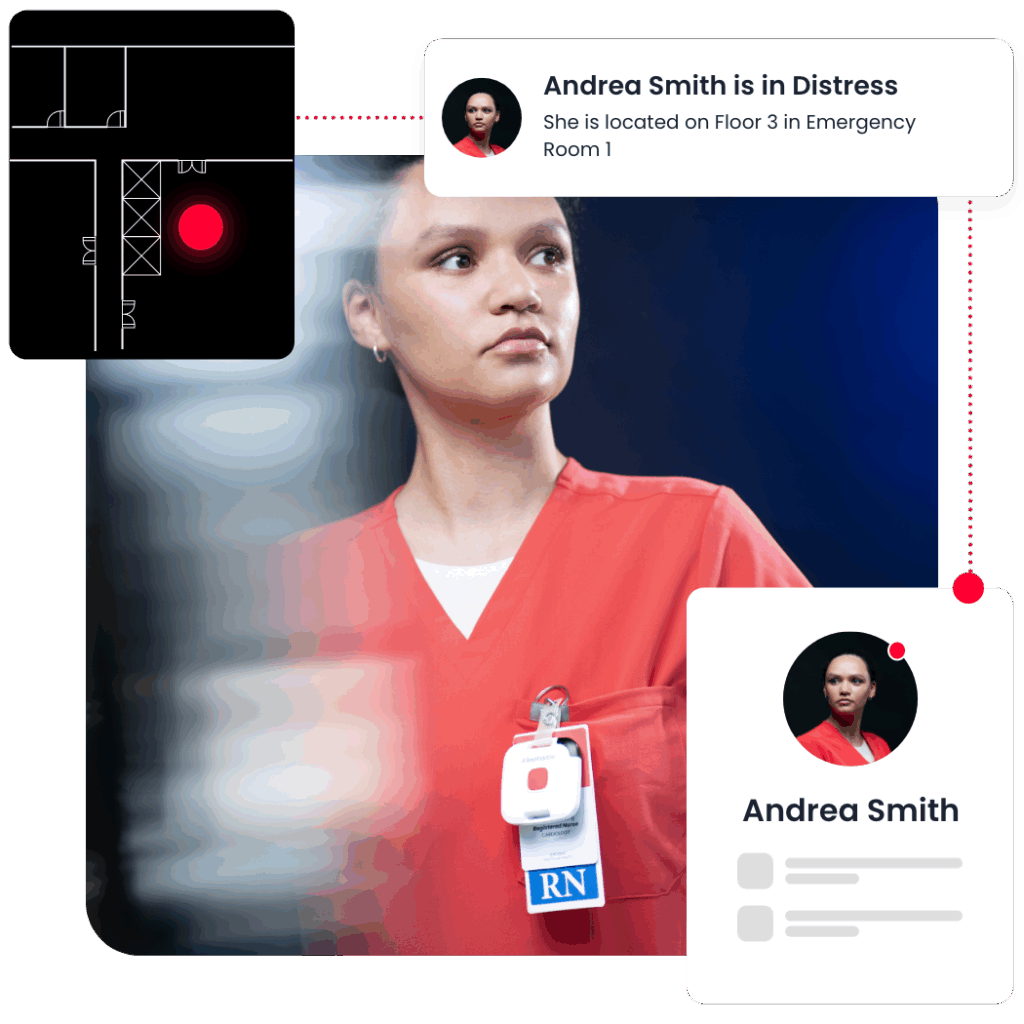
What good looks like: Room-level duress detection with precise location, immediate escalation to trained responders, and post-incident learning.
- How to implement: Standardize response workflows, publish metrics (time-to-first-responder), and communicate improvements.
- Kontakt.io can help: Our smart badges enable one-press duress alerts with room-level certainty and rapid routing to the right team.
- During our 2024 interview with Dr. David J. Shulkin, he emphasized that when leaders deploy staff-safety tools like duress badges, it signals values—and that rapid, successful rollout hinges on clear intent, accountable owners, timelines and resources, clinical buy-in, and transparent feedback loops.
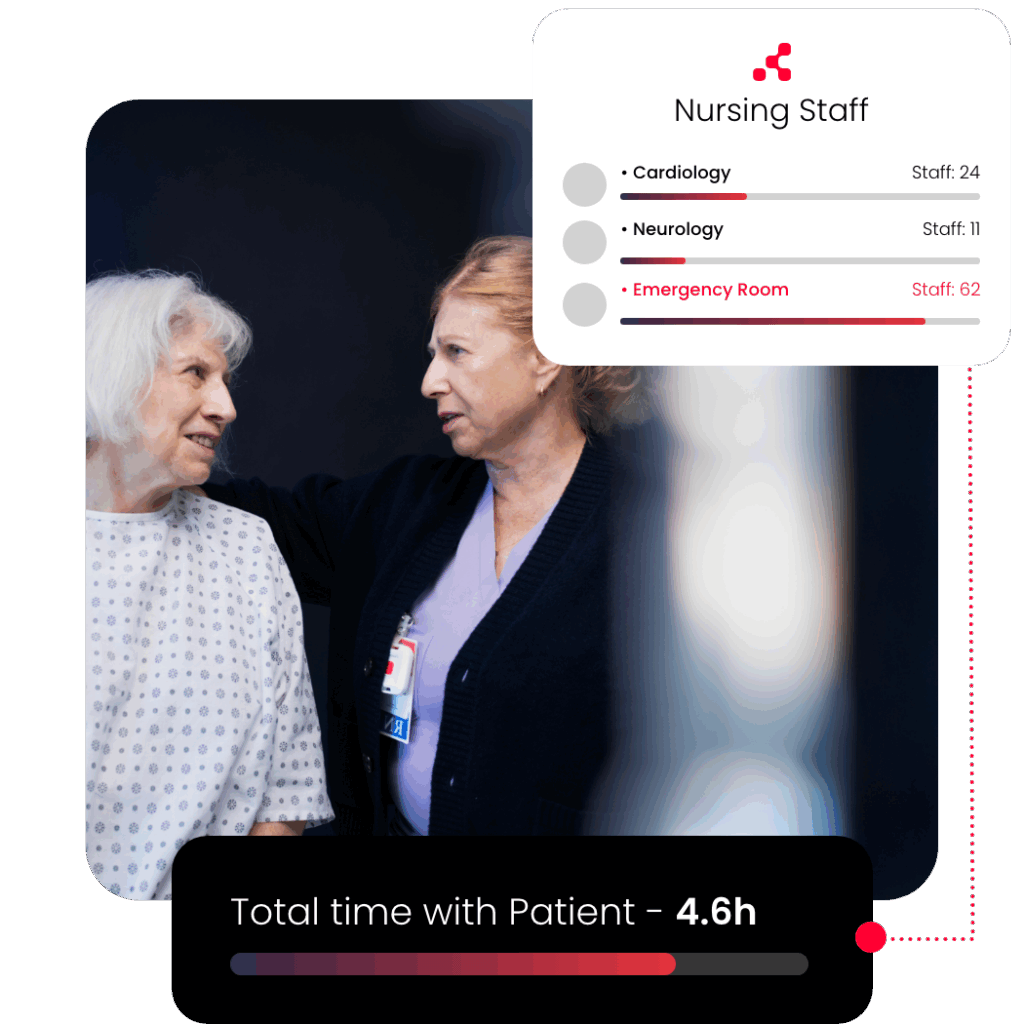
Operational Visibility into Demand and Risk
- What good looks like: Live views of bed status, staffing coverage, and equipment readiness; proactive alerts for OR/ED bottlenecks.
- How to implement: Integrate location signals (RTLS) with EMR schedule data to detect exceptions—late trays, missing pumps, unready rooms—before they hit the patient.
Reduced Manual Burden via Smarter Operations
- What good looks like: Automated discharge triggers, EVS dispatch when a room empties, transport coordination tied to real demand.
- Kontakt.io can help: Our platform automates room turnover events and streamlines mobile medical equipment distribution and recovery.
Leadership Accountability & Feedback Loops
- What good looks like: Regular safety walk-rounds, transparent dashboards, and visible fixes for reported hazards.
- How to implement: Establish a 30-day “report-to-resolution” SLA for safety and workflow issues; share outcomes in huddles.
Data-Informed Prevention vs. Reactive Fixes
- What good looks like: Predict staffing hot-spots and supply-demand mismatches; use trend data to shape schedules and inventory.
- Kontakt.io can help: Real-time signals, analytics, and simple interfaces so leaders can ask, “Where are we at risk in the next two hours?” and act.